Reducing The High Costs
of Chronic Illnesses
In the US, 90% of the $4.5 trillion spent annually on healthcare goes towards managing chronic and mental health conditions. Each disease or condition has its unique decision algorithms, measurements, symptoms, treatments, and outcomes.
Disease-specific tools (e.g., apps), particularly for patients, can play a prominent role in effectively managing complex needs. They can help patients navigate administrative tasks and provide tailored support for their specific conditions. The benefits of improved patient outcomes and reduced healthcare costs are substantial.
The Need to Integrate
Patient Tools
to Manage Diseases
“Freestanding” patient tools are not integrated into decision-making, cannot be used as a communication channel, nor can we easily learn from the data they can collect.
We cannot correlate the data with health outcomes to prove they make any difference.
Moving Towards Value-Based Care Models

New care models, such as value-based care (US), are gaining traction to address the ever-increasing cost of health care. These models directly measure and reward better disease management in a patient population.
The business model of health care itself is changing in a direction that will reward outcomes and the type of disease management our connected tools enable.
A one-size-fits-all approach with one-size-fits-all information systems is no longer sufficient; specialized solutions are needed for more optimal care solutions.
In the short term, our business model and focus are different, but this is the big price available in the end.
reference for picture above www.delveinsight.com/blog/value-based-healthcare-model

Chronic Illnesses Demand Tailored Digital Solutions
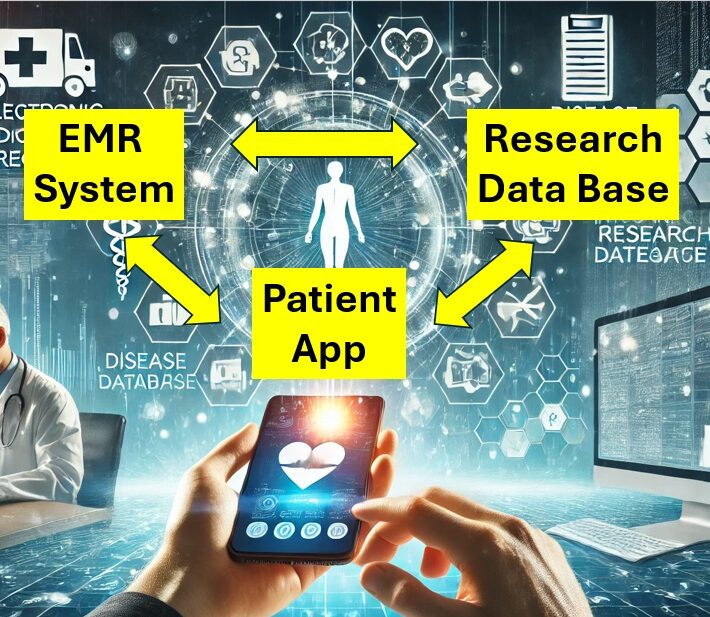
Patients can benefit from more comprehensive, tailored electronic tools, as can researchers from the data collection this enables.
There is also a clear benefit from the additional support that can be offered for expensive medications.
These benefits do not hinge as much on one system, as they do in the communication and exchange of information between the different systems,
Using Obesity as An Example
Below, obesity ais used s an example to illustrate the need and the opportunities for digital health bridges.
The same analysis can be made for most conditions and chronic illnesses.
Opportunity for an Obesity Disease Management System
- Many people are overweight and obese.
- There are severe health implications with many dimensions. Some of these dimensions may not be well managed or measured.
- Intervention requires behavioural change, which is very difficult. Electronic tools can be an effective tool for these interventions.
- There are expensive medications available. The medications are more effective when used with electronic support tools. These tools help provide more long-lasting results.
- Insurers' criteria for usage tightly control access to medication. This requires expensive administrative support.
- Little research exists on how biology and other patient factors affects the effectiveness of medication and behavioural interventions. There is a high need for real-world evidence.
- We need better quality real world evidence to evaluate the long-term outcomes of interventions. This information will be crucial to determine the true value and payers willingness to pay.
Brief Analysis of Existing Solutions
- EMR System: There is perhaps not a compelling need for a disease specific system. Such a system will have to be set-up also to manage complications of obesity which means a more general system.
- Patient App: There are numerous apps. Some are well funded, well recognised, and has developed "state-of-the-art" functionally and user friendliness. Some, i.e. Noom, have established relationships and solutions for providers of GLP-1 medication.
- Connected Patient App: Very few apps are connected to EMR systems. This reduces the ability to communicate, coordinate, and monitor. It also makes the data collected by any app less valuable.
- Research Database for Obesity: SOPHIA, ORBiS, and the VHIR Obesity Sample Bank are examples of significant initiatives. However, the emphasis in this research with less attention to patient tools, patient empowerment, and daily clinical practice. These are also European solutions that may fit better in a single payer system.
- Payer Related Administrative Tools: Some models are available (mainly in the US) but not the type of clinician and patient connected model we propose to reduce complexities and costs. Systems integration to reduce administrative costs still have potential to be developed further.
Obesity Opportunity
While numerous apps address obesity, a complete disease management solution is lacking.
The greatest opportunity lies in connecting patient self-management tools with EMR systems for coordinated care and data collection used in research.
Coordination with payer systems and patient support programs is also crucial and sub-optimal in current solutions.
The focus for research in obesity for a new system should probably be the overall cost-effectiveness of interventions over time in RWE, rather than biology-related research. Noom appears to be well positioned, which is rare for any disease, but it shows the potential of our model.
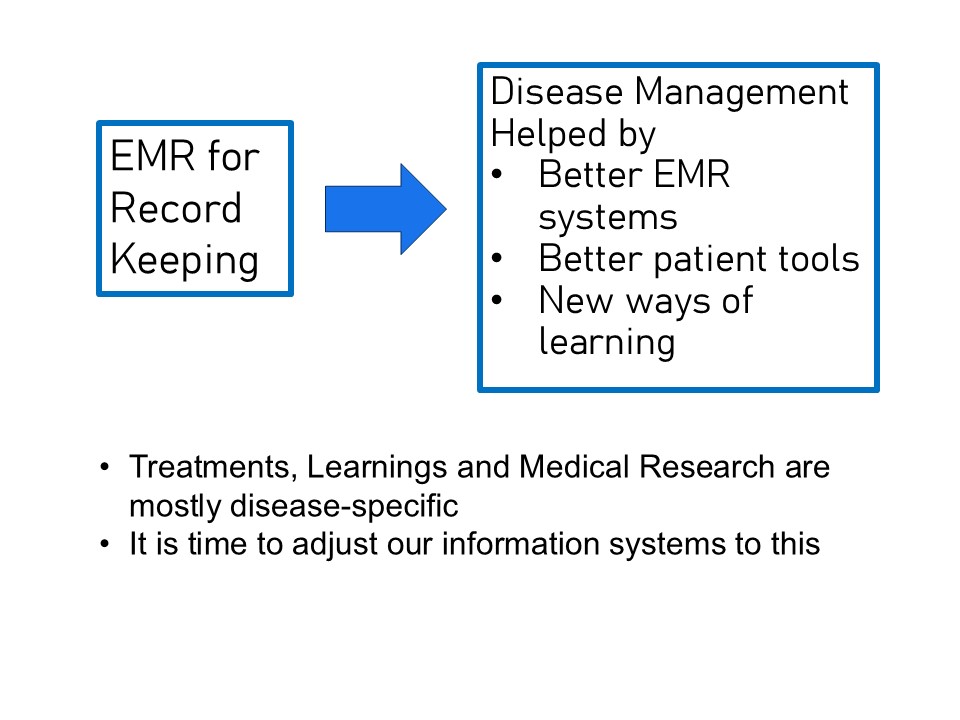
Research & Learnings about Diseases are Almost Exclusively Disease Specific
This is how research is organized. Our gold standard of randomized, double-blind, placebo-controlled studies is far more specific than this, ideally just isolating a single variable in a select population.
There are good reasons for this but this is not what the real world looks like.
The Only System Usually Available - The EMR system is NOT Specific
Few EMR systems were set up to support the type of AI-assisted research that is now possible. They are also seldom designed to optimize disease management or connect with patients.
- Should we expect our systems built for everything also to be an optimal tool for research within specific diseases?
- We call it a “medical record,” but how exactly do we use it to treat our patients? Could our EMR become a better disease management tool?
- How do we best support patients also to remember, understand, and carry through our recommendations?

Medical Research

Medical Specialists
EMR Systems
Connecting a Customized Disease Management App with a General EMR system?
If this was easy, it is likely that it would already be more common. One of the major hurdles is the fragmented base of EMR systems and market dynamics.

Systems: A Complex Challenge
Integrating a disease-specific app and research database with a general EMR system presents significant hurdles.
The challenge isn’t technical; market dynamics and our need to build and protect our intellectual property are crucial considerations.
Existing systems may not be optimal, and collaboration with numerous EMR suppliers is challenging. There are many of them, and they are in control.
If connecting with existing systems were less challenging, we would be happy to do so. However, building proprietary systems is also an option.
Our Own & Integrated Disease Management System
We do not intend to build and sell information systems. Instead, we focus on designing superior services and solutions powered by our unique systems.
We see two main avenues for this approach:
Own Virtual Clinics Optimized for Specific Conditions
By leveraging new systems, we can create highly efficient, specialized clinics. While these could be physical locations, virtual clinics offer a more scalable and adaptable model. Virtual clinics can directly recruit patients online or provide specialist access to general practitioner service providers, enhancing the reach and efficiency of care delivery.Revolutionizing Specialty Pharmacies
Our systems can enable the creation of a new type of specialty pharmacy designed to manage biologics and other high-cost, specialized medications.
By focusing on these two avenues, we aim to drive innovation in healthcare delivery while maintaining efficiency and scalability.
Will Physicians Derive Enough Benefits to Switch Systems?
EMR systems are not particularly complicated, which is why there are so many suppliers. However, they are often deeply entrenched, which means that the benefit of a new system has to be significant to motivate the expense and effort of switching.
Even a paper chart works just fine and is often faster to use. Instead, the main benefit of electronic systems is the ability to exchange information with other personnel and different systems.
Directly involving the patient in this system is a natural extension of this, as is the involvement of patient support programs and insurers.
Once an electronic connection is established, it is only natural to provide the patients with better tools and explore this for research and learning. For the latter, AI is the great new enabler.
However, in most health systems, physicians do not derive a significant direct benefit from better disease management and are unlikely to pay for any new solution. Thus, the real challenge lays in the business models and the lack of direct incentives to improve care.

Creating Virtual & Specialized Clinics
Managing virtual clinics for medical services is an established business model. The clinic owner takes a portion of billings from the medical services provided.
We are just looking to optimize this with state-of-the-art, AI-supported EMR systems, disease-specific patient tools, and taking advantage of research opportunities to manage specific conditions more optimally.
We do so while providing a great working environment for physicians, ensuring enumeration and conditions are competitive.
While the initial model is based on a traditional fee-for-service system, our real target is a future of value-based care. This is where the competitive benefit we develop from optimized learning will be greater.
Revolutionizing Specialty Pharmacies
Specialty pharmacies provide a support system for expensive medications. They offer more than just dispensing. Collaborating with a pharmaceutical company and its patient support program, they work “in the background” to obtain payer approval to fund the medication.
This process depends on communication with many stakeholders, which is very resource-intensive and costly, estimated at 10-15% of the drug’s cost.
There is a significant opportunity to improve these workflows with electronic connections and AI’s assistance.
This and less paperwork and administration may be enough to get clinics to switch systems.

Examples of
Possible Changes

In The Clinic
• The EMR system is prepopulated with information from the patient before any interaction.
• AI will help schedule patients according to estimated time. Patients schedule their own visits.
• Helped by AI, relevant information is shown in a disease dashboard to make it easier to see key data in a snapshot. This may include data entered by patients before the visit, between visits, from the app, or by monitoring devices.
• Your system will enable you to send an AI-generated summary of the visit and the treatment plan to the patient.
• The system can generate suggested prescriptions for you to approve based on the situation, your history of prescriptions, and your preferences. The patient automatically gets a copy of the prescribed information. The same applies for lab requisitions. Both may integrate forward with the pharmacy and the lab for convenience
• The system may suggest useful information for the patient, which can be directed by simply ticking a box. You may set up your system to send this information to all patients with specific conditions. AI will help you organize this over time.
• Additionally, if you think any type of longitudinal data would be useful, you can discuss its collection and get an agreement. Further information and instructions are sent to the patient by ticking a box in your system. The system will allow you to customize the the collection.

For Research
• Improved data collection in EMR systems
• “Prescribed” (physician-initiated) collection of data directly from patients.
• Automated collection of data from a disease management app.
• Donation of tissue or other biological samples. By patients.
Please let us discuss
- What key information would you like at your fingertips to manage your patient’s disease?
- Can or do patients contribute any valuable data or trends? (Above, you simply ask how they are doing or what brings them in.)
- What would be the best way to visualize 1. and 2. in a single snap-shot?
- What do your patients need or want to manage their disease?
- Do you prescribe expensive treatments that require significant paperwork and the help of patient support programs?
